Abstract
Introduction: Air travel may expose patients with sickle cell disease (SCD) to an increased risk of disease related complications. Several factors are felt to contribute, including prolonged hypoxia, dehydration, temperature changes and stress. The Canadian Pediatric Society position statement recommends that SCD patients use supplemental oxygen on flights. While other notable guidelines including the National Heart, Lung and Blood Institute (NHLBI), the National Center for Biotechnology Information (NCBI), the Canadian Haemoglobinopathy Association (CanHaem) and the British Thoracic Society do not make specific recommendations. Since available guidelines and evidence lack consensus, it is unclear what recommendations healthcare practitioners (HCPs) should counsel to their SCD patients.
Objectives:
Determine the recommendations North American hematology HCPs make to SCD patients regarding air travel.
Determine the proportion of HCPs recommending supplemental oxygen to SCD patients.
Among HCPs that recommend supplemental oxygen, determine which patient factors influence their decision.
Evaluate patient experiences regarding supplemental oxygen recommendations prior to air travel.
Methods: First, a literature review using PubMed, TRIP database, Medline (Ovid) search engines was completed. Two investigators independently reviewed abstracts and references. Second, a cross-sectional online survey was circulated through CanHaem (186 members) and the American Society of Pediatric Hematology/ Oncology (ASPHO, 1991 members) listservs. North American hematology HCPs were asked to share their air travel recommendations. The survey was peer-reviewed by 7 practitioners prior to distribution for content and face validity. Similarly, a patient survey regarding experiences with air travel was distributed through the Sickle Cell Disease Association of Canada (SCDAC) listserv. University of Alberta ethics research board approved.
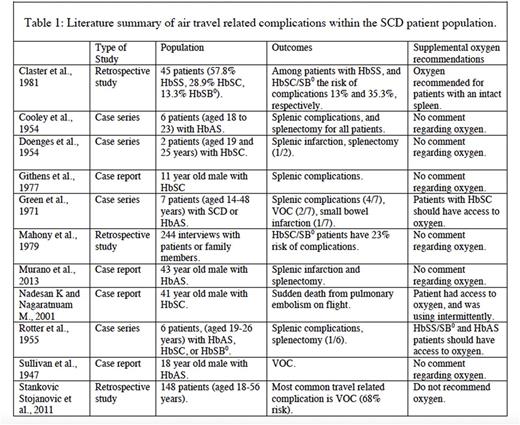
Results: A review of the literature is summarized in Table 1. A total of 81 surveys were returned with 79 evaluable for analysis. Demographic data reveals that most survey respondents are physicians (90%), pediatric providers (77%), and practice at an altitude <100m above sea level (59%). Sixty-five percent practice in USA, and 35% in Canada. Eighty-two percent of HCPs do not recommend the use of supplemental oxygen for flights under any circumstance. Among those recommending oxygen, 9% recommend it for all patients, and 6% for HbSS/SB0 patients only. While most HCPs did not recommend oxygen, they did advise patients to increase hydration (94%), carry analgesics (94%), and wear warm clothes (83%). A few HCPs discouraged air travel altogether (12%). Air travel is considered a risk factor for vaso-occlusive crises (VOC) and acute chest syndrome (ACS) by 67% ad 37% of HCPs, respectively. Among HCPs recommending oxygen, most indicate that a previous history of VOC, stroke, silent infarct, ACS, splenic sequestration, or a history of altitude related complications increase the likelihood of recommending oxygen. Length of flight is an important consideration for HCPs recommending oxygen; 46% recommend oxygen for flights >6 hours, 31% for flights >10 hours and the remainder for all flight lengths. In a small sample of patients (n=5) the majority have experienced a sickle cell crisis during or shortly after air travel. Only one patient participant has used oxygen in the past.
Conclusion: Most HCPs surveyed do not routinely recommend supplemental oxygen to their SCD patients as a prophylactic measure. Among HCPs that recommend oxygen both patient and flight factors influence their recommendations. Although oxygen is not a routine recommendation, most indicate that air travel is a likely risk factor for VOC. In fact, there are numerous published cases of air travel related complications, most commonly splenic complications and VOC, in the SCD population (Table 1). There is a lack of consensus among North American HCPs regarding supplemental oxygen recommendations. Further investigation is needed to delineate the need for supplemental oxygen to prevent complications during air travel for SCD patients.
Bruce: Bristol-Meyers-Squibb - consultant 2016-2017: Consultancy; ovartis consult and ad board 2015-2016: Consultancy; Apopharma 2015: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.